Behavioural Sleep Interventions for Autistic Children

Anita Bennett-Stewart
Behavioural Sleep Specialist & Behaviour Consultant

Sleep difficulties are commonly experienced by all children. In fact, up to 50% of neurotypically developing children experience sleep difficulties.1 However, the prevalence of sleep issues is significantly higher amongst neurodivergent children, with up to 80% of Autistic children experiencing poor sleep.2
Although sleep difficulties are therefore common, this does not mean poor sleep is healthy. Poor sleep has a systemic impact on our quality of life, negatively affecting our mood, information processing, memory and even our safety. Research indicates that sleep difficulties do not resolve on their own as the child gets older. Instead, for Autistic children, sleep difficulties may continue from their early childhood and into young adolescence.3
So how can we help children experiencing poor sleep sleep better?
“Autism is not a life sentence of poor sleep and tired days”
– Dr Gregory Hanley, PhD, BCBA-D
What is Behavioural Sleep Intervention?
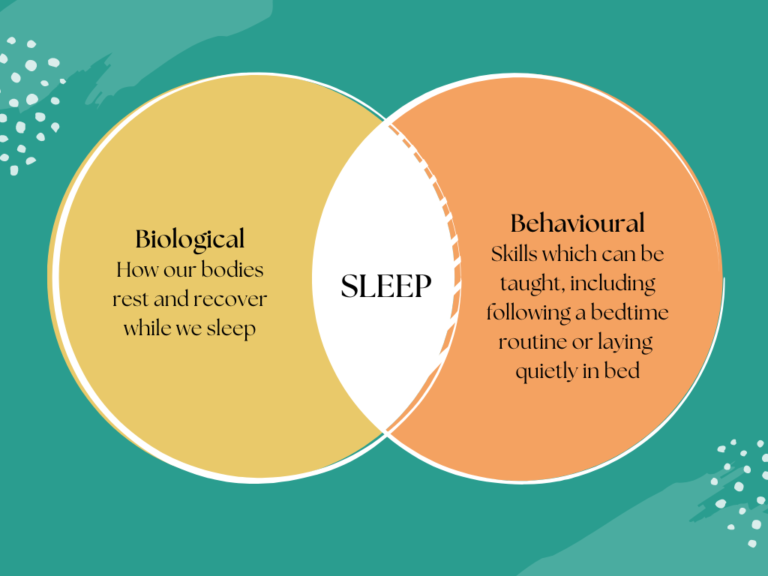
Sleep is both biological and behavioural. While we sleep, our bodies rest and recover. However, following a bedtime routine and laying quietly before sleep are behavioural skills that can be taught. Behavioural Sleep Intervention is teaching a child skills to support a better night’s sleep.
What skills may be addressed in Behavioural Sleep Intervention?
Skills to support a better night’s sleep may include:
- Following a bedtime routine: Some children may become upset during the bedtime routine. Initially Behavioural Sleep Intervention may focus on adjusting the bedtime routine so the child enjoys this routine each evening, or gradually shifting from their favourite activities to brushing teeth to bedtime. For older children, this may look like creating their own bedtime routine and following this independently.
- Laying in bed quietly before sleep: From the time we go to bed, it should take about 15-20 minutes to fall asleep. Learning to lay quietly in bed before falling asleep is an essential skill to healthy sleep habits. However, for many children this can be difficult and they may instead call out to their parent, get out of bed or play in their room. Behavioural Sleep Intervention can support children to learn how to remain quietly in bed before falling asleep.
- Falling asleep at the start of the night: Teaching the child to fall asleep at the start of the night typically involves changes to their current sleep set-up. For example, changing sleep aids to those which the child enjoys and are suitable for the family long-term. Fading old sleep aids and adding new ones can include adjusting items the child is sleeping with, such as fading out sleeping with the iPad to sleeping with a small blanket to hold. This can also involve the consultant working with the family to fade the parents’ presence at sleep time, if the family would like to do so.
- Falling back asleep during the night: We all wake up overnight, but we don’t always remember it because we fall back asleep so quickly! Teaching the child to fall back asleep upon waking overnight often involves maintaining the sleep set-up overnight. For example, if a child sleeps with a blanket but loses the blanket as they move overnight, it will be hard for them to fall back asleep without it. Identifying suitable sleep aids and helping the child to learn to sleep with these throughout the night is an important aspect of Behavioural Sleep Intervention.
- Following an age-appropriate sleep schedule: Sleeping for a consistent amount and at consistent times each night is critical to healthy sleep habits. Reviewing a child’s current sleep schedule is an important first step in Behavioural Sleep Intervention. Then, the consultant will work with the family to identify a new schedule which will be suitable for the family’s routine and ensure the child is sleeping enough each night. Shifting a child’s sleep schedule typically occurs in small adjustments made each night until their ideal sleep time is met.
These are just a few of the important skills which can be taught in Behavioural Sleep Intervention!
How are these skills taught in Behavioural Sleep Intervention?
To help children learn these skills, the consultant will work together with the family to identify what methods are most suitable for the family and their values. Autistic children may require further individualised behavioural supports to acquire these new sleep habits efficiently and effectively. Effective Behavioural Sleep Intervention methods include:
- Reinforcement – Praise and rewards to encourage your child to continue these new sleep habits
- Prompting – Such as reminders and modelling, to help your child as they initially learn new sleep skills
- Communication teaching – Teaching your child to communicate their wants and needs at bedtime without calling out or becoming upset at bedtime
- Shaping – Gradual shifting your child’s sleep routine step-by-step
- Making it fun! – Learning your child’s individual preferences and including these as much as possible so they learn to enjoy bedtime!
This is just the first in a series of articles on Behavioural Sleep Intervention. At Super Kids, we practice Behavioural Sleep Intervention to support neurodivergent children, including Autistic children or those with intellectual disabilities, sleep better. We believe healthy sleep habits can be taught and consistent sleep is achievable!
Resources:
- Jin, C. S., Hanley, G. P, & Beaulieu, L. (2013). An individualised and comprehensive approach to treating sleep problems in young children, Journal of Applied Behaviour Analysis, 46(1), 161-180.
- Richdale, A. L., & Schreck, K. A. (2009). Sleep problems in Autism Spectrum Disorders: Prevalence, nature & possible biopsychosocial aetiologies, Sleep Medicine Reviews, 13, 403-411
- Mazzone, L., Postorino, V., Siracusano, M., Riccioni, A., Curatolo, P. (2018). The relationship between sleep problems, neurobiological alterations, core symptoms of Autism Spectrum Disorder and psychiatric comorbidities, Journal of Clinical Medicine, 7(102), 1-12.
Disclaimer: The advice in this article is general in nature. If your child experiences sleep difficulties, reach out to a trusted professional for further individualised advice and support.
Super Kids acknowledges each individual’s personal preference to use identity-first or person-first language to describe themselves or their loved one. We interchangeably use both language conventions and therefore refer to both Autistic children and children with Autism.